Lina can’t take it anymore. Lately, she’s been having stomach pains more frequently and they are getting worse, especially after big meals. This time, the pain is almost unbearable. After eating fried chicken with her children, she develops the same pain on the right upper side of her stomach.
She feels sick too. It’s time to visit the doctor.
After examining Lina, the doctor tells her that she has acute cholecystitis, which is an inflammation of her gallbladder. On ultrasound, the doctor found the culprit – a gallstone is blocking her cystic duct, a tube that carries bile from the liver and gallbladder to the small intestine.
Now she remembers: three years ago, the doctor told her she had gallstones in her gallbladder, but she didn’t need to have them taken out because they weren’t causing any symptoms.
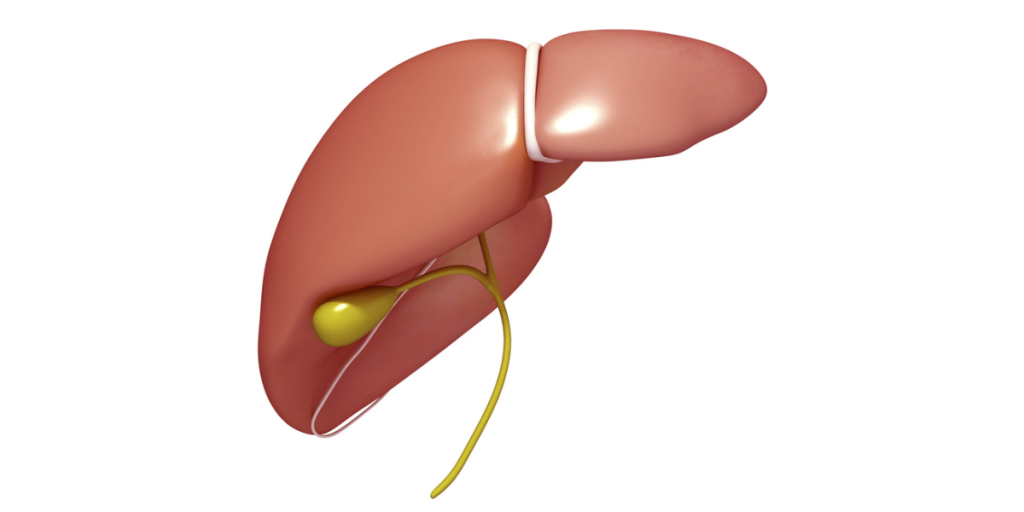
*Caption for image: Here’s a simple diagram showing you the location of the gallbladder and liver. The bile ducts are the green “pipes” which flow bile juices between organs. People sometimes refer to the bile ducts as “the biliary tree” because of their similarity to the branches of a tree.
Although Lina is a fictional character, her presentation is typical of a patient with gallbladder disease.
The gallbladder is a small, pear-shaped organ beneath the liver. It stores bile – a yellowish, brownish-green cocktail of digestive juices that helps in digestion, fat absorption, and getting rid of food waste. Under normal circumstances, when the body detects fats in the food you eat, the gallbladder receives a signal to release bile into the small intestines via bile ducts.
What causes gallbladder disease?
Anything that slows or blocks the passage of bile will result in bile build-up. This can lead to cholecystitis (gallbladder swelling and inflammation), as well as bacterial infection. Gallbladder disease symptoms emerge when inflammation begins; as the blockage and inflammation worsen, so do the symptoms.
Here are some things that can go wrong and cause gallbladder disease:
Gallstones: The most common cause of gallbladder disease. Gallstones within the gallbladder may not cause any symptoms. However, if they migrate to the cystic duct and block bile flow, they can cause inflammation and pain.
Tumour: Bile flow obstruction can happen from a benign polyp within the gallbladder, or a cancerous growth developing in a nearby organ (liver or pancreas). The bile build-up will eventually lead to cholecystitis.
Cholangiopathy (Diseases of the Bile ducts): The main concern with cholangiopathy is the narrowing of bile ducts resulting from inflamed bile ducts. Once more, sluggishness or backflow of bile can lead to inflammation of the gallbladder. Infections, poor blood circulation, autoimmune diseases, genetic causes, or even unknown reasons can cause cholangiopathy.
Acalculous cholecystitis: This is a less common but more severe form of gallbladder inflammation. It happens without gallstones or cystic duct obstruction. Patients who are critically ill, such as those with severe infections, burn injuries, or trauma, are at risk.
How does gallbladder disease present?
Pain is the most common presenting symptom of gallbladder disease, and it usually occurs after eating fatty foods. The pain typically happens in the mid to upper-right sections of the abdomen. It can occasionally spread to the back between the shoulder blades. Doctors describe the pain as “colicky” – a spasmodic, twisting type of pain that comes and goes.
Abdominal discomfort: Bile obstruction can cause disrupted digestion and common symptoms such as bloating, belching, heartburn, nausea, and vomiting.

Changes in stool and urine colour: People with gallbladder disease may notice lighter-coloured stools and darker urine.
Jaundice: Yellow tinge to the skin and eyes indicates bile blockage.
Fever and excessive sweating: These symptoms suggest a severe infection or gallbladder perforation, and they are warning signs that you should seek immediate medical attention because you may require emergency surgery to treat the condition.
I think I have gallbladder disease, what should I do?
Speak to your primary care provider early on if you suspect gallbladder disease. Because the symptoms of gallbladder disease may be similar to some other conditions, you must describe your symptoms and ask questions about the tests to confirm your diagnosis.
Diagnosis of gallbladder disease
Since the gallbladder sits close to other surrounding organs, right-sided abdominal pain can also arise from the liver, pancreas, or digestive tract. After a physical examination, the doctor may order several blood tests and imaging tests to work up your condition.
While blood tests are needed to rule out infection, liver, or pancreatic diseases. The imaging techniques will help in detecting the presence of gallbladder disease, the location of the gallstones, or even obstruction in the bile flow.
Here are some common imaging procedures to work up for gallbladder disease:
- Abdominal ultrasound: This is a simple and non-invasive approach that can detect gallstones and bile blockages with up to 95% accuracy. Fluid accumulations and a thicker-than-normal gallbladder wall also point to gallbladder inflammation.

- HIDA (hepatobiliary iminodiacetic acid) scan: The procedure involves injecting a radioactive chemical into your bloodstream and allowing it to travel through your liver, gallbladder, and small intestines. The camera captures images to show the liver and gallbladder’s functioning and detect issues such as gallstones, inflammation, leakage, blockage, and bile duct problems.
- MRCP (magnetic resonance cholangio-pancreatogram) is a special type of MRI (magnetic resonance imaging) capable of producing detailed images of your pancreas, gallbladder, and bile ducts. Doctors use MRCP to detect stones, tumours, and inflammation in the organs and ducts.
- ERCP (endoscopic retrograde cholangio-pancreatogram) has a similar purpose to MRCP, but it is a more invasive process. Because of this, doctors don’t usually use it just to make a diagnosis nowadays. Instead, they use it for biopsy, removing bile duct stones, or placing stents to improve bile flow.
What is the procedure for removing the gallbladder?
There are two techniques to remove the gallbladder – open surgery and laparoscopic technique. The surgical approach your doctor recommends will depend on your medical history.
Laparoscopic cholecystectomy is now a preferred treatment for most uncomplicated gallbladder diseases. This keyhole surgery is usually performed under general anaesthesia. During the procedure, the surgeon will make a few small incisions on your abdomen, each measuring less than one-half inch.

We can insert a camera and surgical instruments through these small insertions. After removing the gallbladder, the surgeon will stitch the incisions and secure them with small dressings.
This procedure is minimally invasive, resulting in faster healing with a smaller wound. After surgery, patients have shorter hospital stays, lower risk of complications, and better cosmetic appearance than with conventional gallbladder removal.
What are the potential complications of untreated gallbladder disease?
Due to its corrosive nature, bile blockage can cause inflammation of the bile ducts, liver, and pancreas. Here are some possible scenarios:
Cholangitis: When bile ducts experience inflammation, they undergo scarring and constriction, eventually leading to bile obstruction. This condition kick starts a vicious cycle of continuous inflammation and further damages other organs surrounding the gallbladder.
Pancreatitis: Gallstones can sometimes dislodge and clog the pancreatic ducts. This blockage will cause pancreatic inflammation. This medical emergency presents with severe pain and requires immediate removal of the obstruction.
Hepatitis: Liver inflammation is a possible complication; persistent inflammation can progress to hardening of the liver (cirrhosis) or liver cancer.
Gallbladder cancer: Gallstones can slightly increase the risk of developing gallbladder cancer, a rare type of cancer.
What can I expect after the gallbladder removal surgery? Will it affect my digestion?
Post-operative period: Your post-operative hospital stay depends on the type of procedure. With open surgery, you will likely require a longer recovery period; whereas for laparoscopic surgery, you can expect a faster recovery and thus, a shorter hospital stay.
Pain management: Some patients may experience pain following the surgery. With the right painkillers and wound healing, the pain will subside.
Wound care: Larger wounds from open surgery will require more steps in wound care and will take longer time to heal; smaller incisions from the keyhole surgery will require lesser care and heal faster.

Dietary adjustments and digestive health: Most people experience temporary digestive problems after gallbladder removal. We can begin with sips of nourishing fluids and gradually reintroduce solid food into your diet.
Also, we should avoid high-fat meals at first. Our bodies are intelligent; in a few months, they will adapt and we will be able to resume your previous dietary intake with no problems.
Conclusion
Gallbladder disease can sometimes develop without your knowledge, and most symptomatic gallbladder diseases need surgery at some point. So, if you develop symptoms suggestive of gallbladder disease, it is best to seek medical attention early to prevent complications.
Are you nervous about having an operation to remove your gallbladder? Well, worry no more! Laparoscopic surgery has revolutionised gallbladder removal, offering a straightforward and highly successful alternative to traditional surgery. With these recent advances, patients now experience less pain, minimal scarring, and faster recovery times.
References:
https://my.clevelandclinic.org/health/diseases/22976-gallbladder-disease
https://www.webmd.com/digestive-disorders/understanding-gallstones-treatment#091e9c5e80009210-2-6
https://www.webmd.com/digestive-disorders/tests-diagnose-gallbladder-problems