Colorectal cancer is prevalent in Malaysia. It is the second most common cancer among Malaysians and the third most common cancer globally. Approximately 1 in 20 people has a lifetime risk of developing colorectal cancer. Worldwide, it is the second leading cause of cancer death.
What is colorectal cancer?
Colorectal cancer is cancer that starts from the colon or the rectum. It occurs when the cell growth in the lining of the colon or rectum is out of control.
How does it start?
When the inner lining of the colon or rectum starts to grow into a clump of cells, it is called a polyp. There are different types of polyps. Not all polyps are cancerous. However, some may turn cancerous over many years.
Polyps that are suggestive of being cancerous would have features of:
- The size of the polyps: more than 1 cm
- The number of polyps: more than three (3) polyps
- The aftermath of the removal of polyps: dysplasia observed in the colon
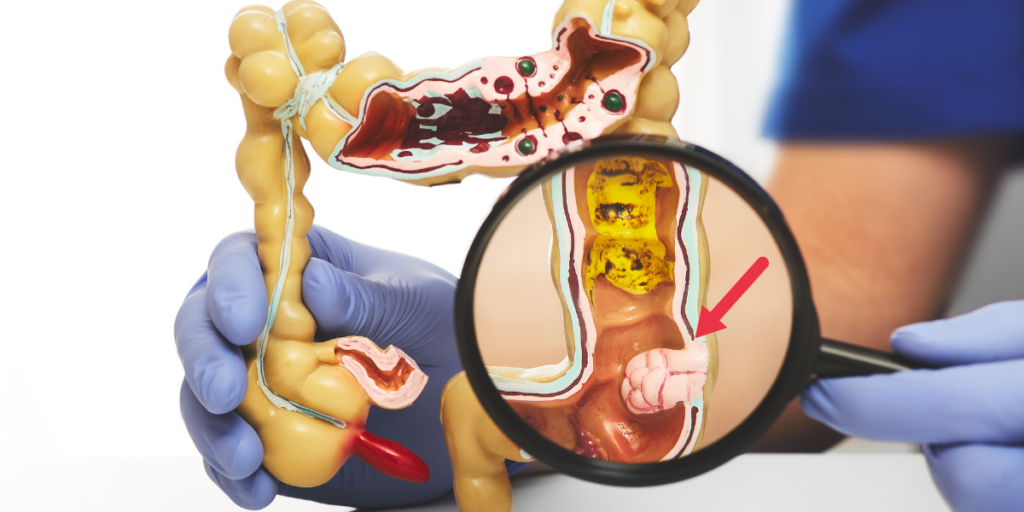
*Dysplasia is a pre-cancerous condition. It is abnormal cell changes within the walls of the colon.
What causes it?
There are no specific causes of colorectal cancer.
Fundamentally, the growth and repair of healthy cells are due to their DNA. DNA is akin to the central control tower of a cell. It usually sends out signals to direct movement within the cells.
When changes occur in the DNA (DNA mutation), the cells no longer listen to instructions. It can lead to uncontrollable cell growth. Normal cells then turn into cancer cells.
Slowly, the cancer cell will start interrupting healthy cell growth and cause the formation of tumours. These cancer cells can also break away from the original tumour and spread to other parts of the body (metastases).
What are the risk factors?
Risk factors do not directly cause colorectal cancer, but they can increase a person’s chance of developing it. Some of these risk factors are controllable, and some are not.
Uncontrollable Risk Factors
Age
Colorectal cancer is usually associated with advanced age. According to the studies, most colon cancers cases involve people above 50 years old. However, there is an increasing trend in the younger population as well.

Gender
Statistics from World Health Organisation (WHO) shows that the rate of occurrence in men (23.4 per 100,000 population) is higher than in women (16.2 per 100,000 population).
According to Malaysia National Cancer Registry (MNCR) 2012-2016, colorectal cancer is the most common cancer among Malaysian men (16.9%) and the second most common cancer among Malaysian women (10.7%).
Race
Based on the Malaysian National Cancer Registry ( MNCR) 2012-2016, out of 100,000 Malaysian population, colorectal cancer was highest among the Chinese (19.6), followed by Malay (12.2) and lastly Indians (11.0). The death rate follows the same sequence.
Family history
Colorectal cancer can run in the family, especially if an immediate family member has been diagnosed with colorectal cancer. The risk increases when more family members have colorectal cancer or the immediate family member have colorectal cancer at a young age.
There are also uncommon inherited conditions in the family, such as Lynch Syndrome (Hereditary Non-Polyposis Colorectal Cancer), Familial Adenomatous Polyposis, Peutz-Jagher Syndrome and so forth.
Inflammatory bowel disease
One may have an inflammatory colon, but it will not always turn into cancer. However, if the inflammatory turns chronic, it might increase the risk of getting colorectal cancer.
Controllable Risk
Unbalanced Diet
Indulging in a particular food, such as processed food and excessive red meat, are associated with an increased risk of colorectal cancer.
Overconsuming these foods can lead to high blood pressure, high blood sugar and high cholesterol. These are associated with an increased risk of colorectal cancer.

Smoke and alcohol intake
People who smoke and consume alcohol are at higher risk.
Inactive lifestyle
People who practice sedentary lifestyles carry a higher risk.
What are the symptoms?
At an early stage, symptoms may not be present. Whenever symptoms are noticeable, it is usually at a later stage.
Here are the symptoms to look out for:
- Blood in the stool or bleeding at the anus
- Continuous belly discomfort (bloated, pain)
- Changes in bowel movement (constipation, diarrhoea)
- Unexplainable weight loss
- Constant feelings of unfinished bowel
- Fatigue
Screening
Screening is crucial to making an early diagnosis.
iFOBT
Individuals with no symptoms but are at high risk (age 50-75) can start with a non-invasive test called the iFOBT.
It is a simple test that collects samples of stools from individuals for lab testing. The presence of non-visible blood in stools may indicate an early sign of cancer. Subsequently, a colonoscopy follows after a positive result.
Colonoscopy
If a person has early signs of cancer, colonoscopy is the modality of choice. A doctor inserts a small tube with a camera attached at the end into the bowels, removing any visible polyps in the process.
Read more about colonoscopy HERE.

CT Colonography
It is considered a virtual colonoscopy. Unlike colonoscopy, it does not need sedation and is a non-invasive procedure. It uses CT scans and X-rays to form 3D images of the bowels.
The process is quick and effective. Individuals require bowel prep (emptying the large intestines) before the procedure. However, a colonoscopy remains a necessity in removing visible polyps.
Computed Tomography (CT)
CT scan produces cross-detailed images through X-rays, looking at extra details like bone structures, soft tissues and tumours. It is an excellent tool to determine a cancer stage. For example, doctors need to ascertain if cancer has spread to the bone, lymph nodes or other organs.
Magnetic Resonance Imaging (MRI)
As the name states, it uses magnetic fields and radio waves to portray detailed soft tissue of the body. Its high contrast resolution image determines whether cancer is present in soft tissues such as the liver.

Treatment
The type of treatment will depend on the exact location of cancer and stage of cancer upon diagnosis.
Colonoscopy
This treatment is used mainly during the early stages of colorectal cancer, where cancer has not gone beyond the colon lining. This procedure can remove any small polyps or any pre-cancerous polyps.
Surgery
The type of surgery depends on the location of the tumour and the stage of cancer. In the early stages, the surgeon can remove the whole tumour. They will also need to remove lymph nodes to check for cancer.
In later stages where cancer has spread to the abdomen, surgery can relieve or prevent complications. In some scenarios, surgery can also relieve symptoms and prolong life.
Chemotherapy
Chemotherapy (chemo) is one of the well-known cancer treatments. It can be in an edible form or given into the vein. Medication flows through the bloodstream to kill rapidly dividing cells, such as cancer cells. The objective is to reduce cancer relapse and slow down the spread of cancer, increasing the survival rate.
Neoadjuvant chemotherapy is chemotherapy before surgery that helps to reduce the size of a tumour. As a result, it is easier to remove the tumour during surgery.
After surgery, doctors may recommend adjuvant chemotherapy. The objective is to destroy any remaining cancer cells. Chemotherapy becomes the primary treatment when cancer has spread too much, and surgery is not an option.

Radiotherapy
Radiotherapy is mainly used for rectal cancer and is quite commonly used in combination with chemotherapy as it increases the efficacy of chemotherapy. Similar to chemotherapy, doctors prescribe radiotherapy before or after surgery.
For advanced cancers, radiotherapy can reduce pain or relieve symptoms.
Targeted therapy
Targeted therapy is a treatment that targets specific genes or proteins that contribute to the growth of the cancer cell.
Immunotherapy
Newer treatment involves immunotherapy, which is a treatment to boost the immune system to fight cancer cells.
Palliative Care
Palliative care is a concept where the treatment plan focuses on well-being support and symptoms management. Cancer is akin to the worst nightmare and news for most people.
Patients face drastic changes, and their mental health will be badly affected. It is essential to have a support system to help them and their family members to cope during the treatment process. Most importantly, palliative care aims to safeguard the patients’ quality of life and assist them to live as dynamic as possible until the end.

Conclusion
The 5-year survival rate for colorectal cancer depends on several factors but is mainly affected by the stage upon diagnosis. The 5-year survival rate is above 80 per cent in Stages I-II.
Therefore, prevention and early detection are crucial. Live a healthy lifestyle have a more balanced diet. Preferably high fibre food like vegetables and eat lesser processed food.
Concurrently, we should monitor for any symptoms and consider getting screened, especially if there are risk factors. Do consult a doctor for a more thorough and detailed explanation of the screening procedures available.
Reference:
- https://www.nst.com.my/news/nation/2021/10/736871/more-66000-malaysians-be-diagnosed-cancer-annually-2030
- https://www.webmd.com/digestive-disorders/picture-of-the-intestines
- https://www.mayoclinic.org/diseases-conditions/colon-cancer/symptoms-causes/syc-20353669
- https://www.cancer.org/cancer/colon-rectal-cancer/about/what-is-colorectal-cancer.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5081307/
- https://cancer.org.my/get-ahead/cancer-care/palliative-end-of-life-care/